Editor’s note: The COVID-19 pandemic remains a constantly changing situation. Accordingly, SIU members are encouraged to check the union’s website and stay in touch with the halls for the latest information. There is a prominent COVID-19 section on the home page at www.seafarers. org. For major announcements, the SIU also sends text alerts linking to the web posts.
As pandemic-related restrictions started to loosen across the United States, the SIU cautiously and deliberately reopened its hiring halls and announced plans to resume classes at its affiliated school in Piney Point, Maryland.
Many states began advancing to different phases of reopening from late May to mid- June. However, the COVID-19 pandemic remained a massively serious threat – as of June 15, at least 114,000 people had died from the coronavirus in the U.S. and more than two million cases had been reported.
Following are some of the major developments since publication of the June edition of the LOG:
- A crew member from the USNS Leroy Grumman, which is part of the SIU Government Services Division fleet, became the first known American mariner to die from the coronavirus. Though not a union member, Joseph Bondoc was part of the unlicensed crew. He was one of more than 20 crew members diagnosed with COVID-19 while the vessel was in a Boston shipyard. A contractor from that same yard also died from the virus.
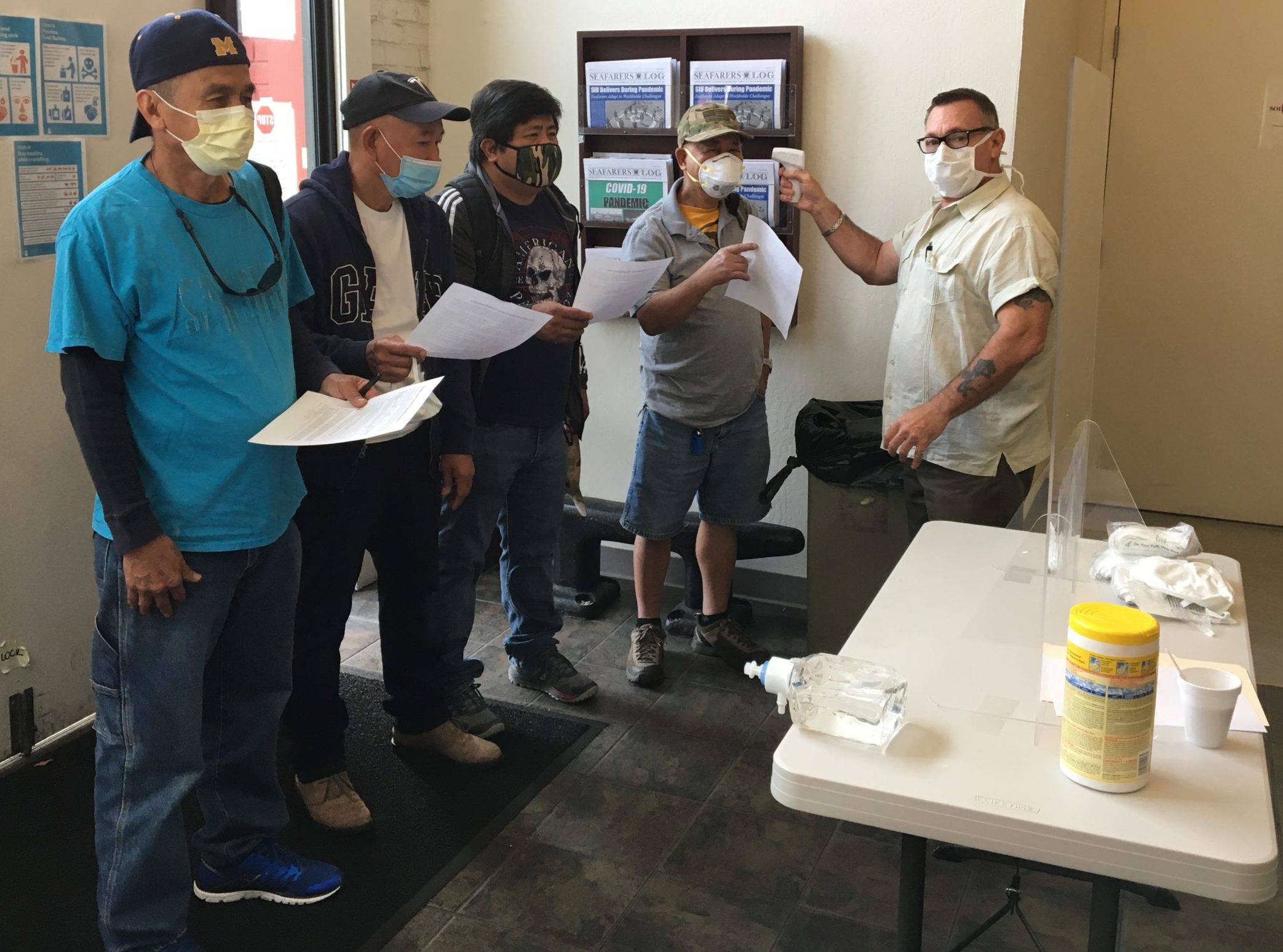
- SIU hiring halls reopened June 15, with numerous safeguards. Vessel servicing also resumed on June 15, wherever allowable, and union headquarters (located in Camp Springs, Maryland) transitioned from a skeleton crew to fuller staffing in all departments.
Pandemic-related modifications have been made at the halls, including extensive cleanings, installation of dividers, shipments of PPE for members and staff, rearranging seats to promote social distancing, and more. Members are required to wear a face covering when entering the building. (A limited number of masks are available at the halls.)

Members return to the Jacksonville hall on June 15
Additionally, visitors must bring a completed medical questionnaire (available HERE) with them when they arrive at a hall.
Similar protocols and precautions are in place at headquarters.
In an effort to keep the numbers down in the halls during this transition of reopening, members should be aware that even after June 15, registration and reclaims are still being done by phone, temporarily. Regular job calls take place for rotary shipping, and general business can be conducted at the halls (filing for vacation benefits, beefs, etc.).
- The SIU-affiliated Paul Hall Center for Maritime Training and Education, in Piney Point, Maryland, is scheduled to reopen Aug. 1. An array of safety-related modifications are being implemented.
Initially, the school will offer a limited number of upgrading courses, with reduced class sizes. The full course content will be presented in a shorter-than-usual period, in order to get students in and out more quickly. Apprentice training will resume in September.
At least during the initial reopening period, students must remain on campus for the duration of their respective courses (including weekends). Students are asked to pack and prepare for their time at the school just as if they were heading to a ship. The school does not have a firm timeline for this policy, but envisions it as temporary.
The original course schedule for 2020 has been completely scrapped. New course dates are available on the SIU website and will be published in the Seafarers LOG. Course dates will continue to be added.
Many steps are being taken to help ensure both functionality and safety. Meal periods will be assigned, altered and staggered. Class starting times will be altered to help promote social distancing. No family members or guests should come to the school until further notice. Gym access will be limited.
The following courses will be offered beginning in August: Able Seafarer Deck; Certified Chief Cook; Chief Cook Assessment Programs; BT Revalidation; Chief Steward; Government Vessels; and BT/Advanced Firefighting Revalidation.
Those with questions should contact the admissions office by phone at (301) 994- 0010 (8 a.m.-4:30 p.m., Eastern Time), or by email at [email protected].
- Crew changes have been among the largest challenges of the pandemic, particularly for the SIU-crewed “shuttle” ships that normally remain overseas. Nevertheless, significant progress was happening at press time.
In late May, SIU President Michael Sacco and the presidents of five other U.S. maritime unions contacted the U.S. Secretary of State and the U.S. Secretary of Defense with an urgent call to facilitate overseas reliefs for American mariners. Signing the letter were Sacco; AMO President Paul Doell; MEBA President Marshall Ainley; MM&P President Don Marcus; SUP President Dave Connolly; and MFOW President Anthony Poplawski. The letter – which was far from the SIU’s lone effort – reads in part, “Scores of U.S. mariners are presently trapped aboard cargo ships, unable to take leave or return home due to extreme COVID-19 lockdown measures imposed by foreign governments. This humanitarian crisis, if not resolved as soon as possible, may threaten the essential supply chain for some 200,000 active U.S. military personnel now serving overseas. The cargo carried on these U.S. flagged ships supports our troops, our allies and the global economy.
“Ship’s captains, officers and crew members who sail under the American flag and perform these essential functions for our country have not been able to set foot on dry land in months. Their workplaces have become floating prisons. Crew members are in danger of losing access to life- sustaining medicines. In many cases, they cannot contact their loved ones at home in the United States as some of these vessels lack Internet access.
“It is well documented that isolation and excessive time serving aboard ship can create increased fatigue and psychological stress, raising the risk of marine accidents. Thousands of mariners across the globe who work on foreign-flagged vessels are in the same predicament.” (The full text of the letter is available on the SIU website.)
The SIU also is actively coordinating with vessel operators, U.S. embassies, the International Maritime Organization, International Labor Organization, World Health Organization, and directly with the host nations to expedite crew changes.
Meanwhile, several SIU-contracted vessel operators chartered a plane to make crew changes in Diego Garcia. That plane returned to the U.S. in late May after the changes were made.
Pre-boarding quarantines largely have become the norm, regardless of vessel location. With that in mind, the SIU in late May posted a message to the membership noting, “It’s extremely important that all members adhere to the agreed-upon protocols prior to joining a ship. This applies whether you are self-isolating at home or in a hotel. While we are navigating these uncharted waters, think of the pre-boarding safety regimen as your part of helping ensure the vessel’s crew remains COVID-free. And remember that if you fail to comply, you are affecting not only yourself but your future shipmates and the fellow members who are awaiting reliefs.”
- The July membership meetings have been cancelled, but plans are being made to conduct the August meetings, with safety measures.
- The U.S. Coast Guard’s National Maritime Center (NMC) on June 4 announced several additional extensions for various documentation. Merchant mariner credentials (MMC) and medical certificates (national endorsements only) that expire between March 1, 2020 and Sept. 30, 2020 are extended until Dec. 31, 2020. Mariners who are actively working on expired credentials that meet the expiration criteria must carry the expired credential with a copy of the NMC notice, which is posted in the Latest News and COVID-19 sections of the SIU website.
The agency also announced that MMCs with STCW endorsements that expire between March 1, 2020 and Sept. 30, 2020 are extended until Dec. 31, 2020. The same is true for STCW medical certificates that expire between March 1, 2020 and September 30, 2020.
###





Comments are closed.